GENERAL MEDICINE E-log
NAME: A sanvith
Roll no: 09
A CASE OF ACUTE CVA PRESENTED IN SUMMER 2023
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and providing treatment best to our skills and wisdom.
A 70 years old male farmer by occupation presented to the casualty with complaints of weakness of right upper and lower limb.
Date of Admission: 08/09/23
CHIEF COMPLAINTS
Weakness of right upper and lower limb since 4 days( 8/9)
Inability to talk since 4 days(8/9)
Patient was apparently asymptomatic till last Friday afternoon (8/9/23). He had his lunch around 12pm after which he called his grandson and after which his speech got slurred . He observed marked weakness in right upper and lower limbs and was not able to get up from the bed. Family members thought it to be simple weakness due to old age so they ignored it. They used diapers for urine and stool. Next morning (9/9/23) weakness persists and he was not able to talk so they came to our hospital.
Weakness was sudden in onset non progressive. No aggravating or relieving factor.
Slurring of speech was sudden and progressed to inability to talk.
H/o Drooling of saliva
H/o hiccups
No h/o deviation of mouth
No h/o involuntary movements, bladder and bowel incontinence
No h/o loss of consciousness
No h/o breathlessness , cough, fever, palpitation, reduced urine output and vomiting.
HISTORY OF PAST ILLNESS
Patient had similar complaints 1 year back for which he took medication for 3 months and as symptoms got improved he left the medicine.
K/c/o CVA (left hemiparesis) 1year back
K/c/o HTN since 2 years
N/k/c/o Diabetes, epilepsy, TB, Asthma
DRUG HISTORY
tablet amlodipine 5mg
tablet atenolol 50mg po/od
PERSONAL HISTORY
➤Occupation: Farmer
➤Patient is married .
➤Patient takes mixed diet and has a normal appetite.
➤Bowel and bladder movements are normal
➤No known allergies .
➤Addictions - Consumes alcohol regularly
General Examination
➤Pallor : not seen
➤Icterus : not seen
➤Cyanosis : not seen
➤Clubbing : not seen
➤Lymphadenopathy : not seen
➤Edema : not seen
VITALS
➤Temperature : 98.2℉
➤PR : 74 beats per minute
➤BP : 160/90 mm of Hg
➤RR : 20 cycles per minute
➤SpO2 : 98% in room air
➤Blood Sugar (random) : 269mg/dl
SYSTEMIC EXAMINATION
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
➤Speech : Impaired
➤No signs of meningeal irritation
Motor system
Tone:-
Rt UL - Hyper
Rt LL-Hyper
Lt LL-Hypo
Lt LL- Hyper
Power:-
Rt UL - 0/5 Lt UL-2/5
Rt LL - 0/5 Lt LL-2/5
Reflexes:
RIGHT
Biceps: ++
Triceps: ++
Supinator: ++
Knee: ++
Ankle: ++
Plantar: Extensor
LEFT
Biceps: +++
Triceps: ++
Supinator: ++
Knee: +++
Ankle: ++
Plantar: Extensor
Involuntary movements - absent
Fasciculations - absent
sensory text cannot be elicited
Cerebellum -
Finger nose test , dysdiadochokinesia, Rhomberg test could not elicited.
Autonomic nervous system - normal
• Meningeal sign
Neck stiffeness -absent
Brudzinski sign -absent
Kernigs sign - absent
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
➤Trachea is in midline.
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid
➤Equal movements in all the quadrants.
➤No visible pulsation, dilated veins and localized swellings.
PALPATION
➤Liver , spleen not palpable.
➤No tenderness
PROVISIONAL DIAGNOSIS : RIGHT HEMIPARESIS
RECURRENT CVA WITH K/C/O HYPERTENSION SiNCE 2 YEARS
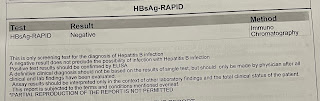
INVESTIGATIONS :
1. Haemogram
9/09/23 10/09/23
Hb ; 13.4 13.3
TLC : 11,000 14,300
Platelet count : 3.18 3.1
PCV : 38.4 38.3
3. Serum Creatinine - 1.3
4. Serum Na+ - 131
5. Serum Chloride - 98
6. Serum Calcium - 1.14
7. Blood urea - 41
8. RBS - 210
TREATMENT
1) Ryle's tube feeding - 2nd hourly water and 4th hourly milk
2) Ecosporin - AV 75 mg/hr PO OD
3) Atenolol 50mg
4)Physiotherapy
No update

Comments
Post a Comment